Precision Medicine for Kids: Tailoring Treatments in Childhood Cancer
September 2024 marks the fifth annual observance of Childhood Cancer Awareness Month, since its official recognition in September 2019. During this month, advocacy organizations, healthcare institutions, research organizations like TFS CRO (Contract Research Organization), patients and their families join together to raise awareness and funds for supporting pediatric cancer clinical research. In the United States (US) alone, approximately 15, 000 children and adolescents are diagnosed with cancer each year, with the most common types including Hodgkin lymphoma, acute lymphoblastic leukemia, neuroblastoma, and Wilms tumor, among others. Although childhood cancer mortality has decreased over the past 40 years, cancer is still the leading disease-related cause of death among children and adolescents aged 1 to 19 years in the US.
Generally, pediatric cancers are rare in the population, which presents a unique set of challenges for clinicians, patients, and their families because the availability of effective treatment options is often fairly limited. However, like with other rare diseases, precision medicine presents valuable opportunities in pediatric oncology to deliver individualized care tailored to each child’s needs. This article will delve into the multifaceted difficulties of treating childhood cancers, highlighting five key challenges, as well as explore how precision medicine is driving advancements in this therapeutic area. Read on to learn more about tailoring treatment in pediatric cancer!
Five Key Challenges Associated with Treating Childhood Cancer
In the last 40 years, the death rate from pediatric cancer has dropped by 70% (ages 0-14 years) and 64% (ages 15-19 years). However, despite this, several obstacles continue to face patients in this vulnerable population throughout their journey from diagnosis to treatment, including the following.
1. Underdiagnosis and Treatment Access Inequities in Socially Disadvantaged Children
In a 2019 model-based study estimating global childhood cancer incidence, Ward and colleagues found that nearly one in two (43%) children (aged 0–14 years) with cancer never receive a diagnosis. However, they found this value varied substantially across global regions, with the highest proportion of cases being missed in low- to middle-income areas. For example, compared to an underdiagnosis rate of 3% for cases of childhood cancer in western Europe and North America, an alarming 49% to 57% of cases were missed in south Asia and western Africa, respectively.
This aligns with the World Health Organization’s (WHO) report that only 30% of children in low- or middle-income countries survive, compared to over 80% in high-income countries. These socioeconomic and geographic disparities likely play a considerable role in the therapeutic landscape of childhood cancer, potentially contributing to limited treatment availability in socioeconomically disadvantaged regions, partially due to an underrepresentation of lower income children in pediatric cancer clinical trials. Of the 6.7 million cases of childhood cancer expected to emerge globally between 2015 and 2030, Ward and colleagues estimate nearly 2.9 million cases will not be diagnosed.
2. Lack of Funding for Pediatric Cancer Clinical Research
Another significant challenge in the field of childhood cancer research is the lack of adequate funding. Research for children with cancer, especially for those with sarcomas and brain cancer, lags nearly two decades behind their adult counterparts, primarily due to pediatric cancers receiving only a fraction of the research dollars granted to adult cancer. Until recently, only 4% of the US federal cancer research budget was allocated specifically to cancer in children. Although the budget allocation is now estimated to be closer to 8% due to broader definitions and more overall funding, there is still a desperate need for increased funding in pediatric oncology clinical research. With the lack of federal research dollars hindering momentum in pediatric cancer research and drug development, pediatric oncologists and researchers must instead rely on funding from private foundations, like the Children’s Cancer Foundation, or large institutions like the St. Jude Children’s Research Hospital to support their research.
3. Limited Patient Population for Childhood Cancer Clinical Trials
One of the key reasons for the limited therapeutic landscape in pediatric cancer is the small size of this patient population, considering childhood cancer is generally rare. In addition to the lack of funding for this type of clinical research, which could otherwise support more treatment advancements, pharmaceutical companies are often less incentivized to invest in testing experimental therapies in children because the population is too small. With a limited pool of potential participants to enroll into childhood cancer clinical trials, researchers face numerous complications in the process of gathering statistically significant data, which is otherwise essential for validating new therapies. Recruitment is challenging as it is even in adult clinical trials for ubiquitous conditions like hypertension or type 2 diabetes, but in children, they are even more potent. The variability of cancer not only further fragments the available pool of potential participants, additional challenges associated with testing drugs in children prolongs the time needed to complete clinical trials and slows the introduction of novel therapies for pediatric cancer.
4. The Recruitment Sensitivity of Pediatric Cancer Populations
There are several ethical considerations researchers must be aware of when it comes to conducting pediatric cancer research. The process of recruiting children into cancer clinical trials requires a delicate balance between the necessity of advancing scientific knowledge and the imperative to protect vulnerable patients. Specifically, informed consent becomes more complex with childhood cancer clinical trials because researchers must obtain consent from the parent/guardian, as well as assent from the child when possible. The consenting process itself is also a sensitive area because ensuring that families fully understand the potential risks and benefits of participation can be an emotionally difficult conversation. Another factor to consider when recruiting children with cancer is the emotional toll that a child’s diagnosis has on their family, often resulting in understandable hesitation or fear with enrolling them in an experimental study. Conducting pediatric cancer research is already challenging, but the ethical and emotional factors affecting this process also contribute to the slow nature of developing new therapies for kids with cancer.
5. Pediatric Cancer Physiology Presents Complexities for Developing Novel Therapies
The physiology of cancer in children often differs significantly from that in adults, which makes the process of researching and developing new effective therapies that much more complex. Children and adults have distinct tumor biology, with pediatric tumors often having comparatively different genetic and molecular profiles. Furthermore, children’s bodies are still developing, making them more susceptible to the adverse effects of cancer treatments such as chemotherapy and radiation. Whereas these treatment approaches are considered gold standard in many types of adult cancer, their use in children raises significant concerns about their tolerability of these treatments and the potential for long-term health complications, including secondary cancers and organ damage. Overall, these differences with pediatric cancer physiology necessitate targeted approaches with precision medicine to deliver individualized care to each child.
Precision Medicine Offers New Opportunities in Treating Childhood Cancer
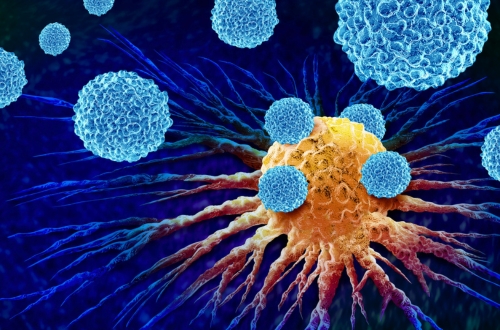
Precision medicine tailors treatment to the individual characteristics of each patient, including the molecular and genetic makeup of their cancer, and it has shown promising potential as a treatment approach for childhood cancers that were otherwise untreatable with standard therapies. Precision medicine has been made possible with the emergence of next-generation sequencing (NGS), which is an advanced technology that thoroughly analyzes a patient’s cancer genome and identifies specific genetic abnormalities that are driving tumor growth. In pediatric oncology, NGS has revealed that over 65% of children with high-risk cancers have tumors with several potentially targetable molecular abnormalities, paving the way for developing new targeted therapies designed to specifically inhibit these tumor growth drivers in pediatric cancer.
Recent Achievements in Precision Medicine Research for Pediatric Cancer
As of December 2020, several large-scale national pediatric precision oncology programs have been initiated, enrolling over 3000 children, adolescents, and young adults (AYA) in the last decade. These programs span multiple countries, including the US, Canada, France, Germany, the Netherlands, the United Kingdom (UK), Korea, and Australia.
A study published April 2024 in Nature demonstrated a pioneering functional precision medicine (FPM) approach that combines genetic testing with drug testing on tumor samples. The study showed 83% of children with relapsed or refractory pediatric cancer treated with FPM-guided therapy experiencing significant improvements in progression-free survival and objective response rate compared to the non-guided treatment group.
More recently, in June 2024, promising results were released from the world’s first study into precision medicine for high-risk childhood cancer. In the study, published in Nature Medicine, precision medicine was shown to be superior to standard or non-guided therapy, both in terms of clinical response and survival. Following an observation period of at least three years after receiving their treatment, 55% of children treated with personalized medicine achieved complete or partial remission, or had their disease stabilized for at least six months. To further underscore why these results are promising, it should be noted that the 384 enrolled participants were diagnosed with highly aggressive pediatric cancers that had failed to respond to previous standard therapy in many cases.
Both studies demonstrate exciting advancements in implementing precision medicine more fully when treating pediatric cancers, specifically by utilizing detailed genetic analyses of the driver genes in a child’s unique tumor biology to guide drug recommendations. This ongoing shift in the therapeutic landscape for childhood cancer, involving moving away from traditional palliative and/or standard therapies to adopt more personalized therapeutic regimens, is showing significant promise for the future in improving the chances of survival in children with high-risk cancers.
Conclusion
In conclusion, although there have been valuable strides in reducing childhood cancer mortality rates, there are still several challenges facing effective treatment and research in this therapeutic area. In response to the several obstacles facing the process of developing and testing new therapies for childhood cancer, precision medicine is offering new hope, providing personalized therapeutic approaches that are tailored to the unique genetic and molecular profiles of pediatric cancers. As we approach Childhood Cancer Awareness Month this September, organizations like TFS and St. Jude are dedicated to continuing to raise awareness and advocate for increased funding and research. By doing so, we can work together to help accelerate the development and implementation of innovative treatments in pediatric oncology, ultimately improving the prognosis and quality of life for children battling cancer.
Support Childhood Cancer Awareness Month This September with TFS CRO
Every September, the St. Jude Children’s Research Hospital holds the St. Jude Walk/Run, a nationwide, 5K-hybrid cancer walk event, that takes place in person and virtually. Scheduled for September 28, 2024, this nationwide, family-friendly event brings together communities to support the lifesaving mission of St. Jude: Finding cures. Saving children.® TFS Oncology CRO is excited to participate in the St. Jude Walk/Run event, in addition to hosting an in-person event in North Carolina, inviting local employees to join us for a day of unity and purpose. Remote TFS employees are encouraged to participate in their local chapters’ events or virtually through the St. Jude Walk/Run mobile app.
Visit the St. Jude Children’s Research Hospital website here to learn more about the St. Jude Walk/Run and discover why St. Jude matters to your community.
TFS Oncology CRO: An Industry Leader in Supporting Pediatric Cancer Research
TFS HealthScience’s Oncology and Hematology services are dedicated to providing comprehensive support for your childhood cancer clinical trials, in collaboration with our TFS Pediatrics team. With a proven track record of over 300 cancer-related clinical trials across all phases, we’re committed to delivering solutions that match your needs. Our global operations teams are fully experienced with navigating the complex landscape of cancer clinical research, offering rigorous operational oversight and adherence to global standards under the strong leadership of Kris O’Brien, VP, Head of Oncology & Rare Diseases at TFS. Visit our oncology CRO website to learn more or connect with a TFS representative here!
Connect with Us
Contact us today to discover how TFS can be your strategic CRO partner in clinical development.